|
HEMOROİD NEDİR?
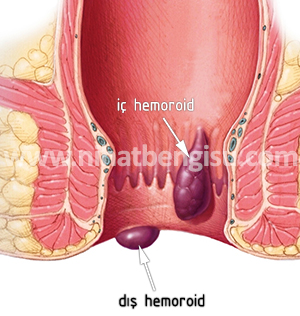
Halk arasında basur olarak bilinen hemoroid anüs ve rektum hastalıklarının başında yer alır. Anüs ve rektum, boşaltım sisteminin çıkış kapısı olup yaklaşık yirmi çeşit hastalığın görülebildiği ve pek çok hastalığın da indirekt belirtilerinin izlenebildiği yerdir. Bu bölgenin hastalıklarına proktolojik hastalıklar ve proktoloji ile ilgilenen hekimlere de proktolog denir. Hemoroid, anüs içindeki hemoroidal toplar damarların zaman içinde anormal genişleyip kırmızı ve mor torbalar (memeler) şeklinde dışarı sarkması, (Resim 1 ve 2) bazen aşınıp delinerek dışkılama sırasında sık sık, parlak kırmızı kanamalar yapması, bazen memelerin aniden pıhtı ile dolup şiddetli ağrı, ödem, iltihaplanma, yaralanma ve ağrı yapmasıdır.
HEMOROİDİN OLUŞMA SEBEPLERİ
|
|
|
Resim 1: Hemoroidlerin şematik oluşumu.
|
En yaygın sebeplerden birisi kabızlıktır. Ayrıca, kolit, proktit, enterit gibi barsak enfeksiyonları, alkol, tahriş edici aşırı acılı gıda tüketimi, yetersiz hijyen, anüs içi hemoroidal damar duvar yapısının doğuştan zayıf olması veya sonradan zayıflayıp torbalanması, prostat büyümesi, tuvalette uzun süre oturmak ve aşırı ıkınmak, gün boyu oturmak veya ayakta kalmak, aşırı yorgunluk, portal hipertansiyon, hamilelik, myoma uteri, over kisti vb. gibi karın içi büyük urlar, kronik ökrürük, şişmanlık gibi karın ve damar içi basınçlarını artıran başka hastalıklar diğer sebepler arasında sayılabilir.
HEMOROİD ÇEŞİTLERİ VE TEDAVİSİ
Hemoroidler öncelikle iç (internal) ve dış (eksternal) olmak üzere ikiye ayrılırlar. Hemoroidlerin çoğu iç hemoroid olup bunlar 4 derece olarak sınıflanır. Ayrıca basit ve komplike; tromboze, akut ve kronik olmak üzere alt sınıflara ayrılırlar.. Anüsün dış kenarındaki eksternal hemoroidal damarların aniden noktasal, tarzda cilt veya mukoza altına kanamaları ve pıhtı oluşturmaları da bir başka hemoroid çeşidi sayılabilir.
|
 |
|
Resim3:Anoskop ile görülebilen grade 1 hemoroid.
|
1) Grade I (1. Derece) Hemoroidler: Hemoroid memesinin yukarı konumda kalıp, anüs dışına çıkmayıp ancak anoskop ile içeriye girildiğinde görülebilmesi halinde 1. derece hemoroid söz konusudur. Kendini sadece kanama ile belli eder. Bu memeler genellikle ağrısız olup, 1 cm'den daha küçük boyutlu, gergin ve ince duvarlı kanamaya hazır iç memeler şeklindedir ve ele gelmezler
TEDAVİ:
1. derece hemoroidler lastik bantla bağlama, sklerozan ilaç enjeksiyonu, halk arasında LASER olarak bilinen infirared ışık koagülasyonu gibi konservatif tıbbi yöntemlerle tedavi edilebilir; ameliyat gerekmez. Bazan sadece melhem, uygun diyet, ılık su oturma banyosu ve istirahat yeterli olabilir. Ancak hazırlayıcı sebepler araştırılıp onlar da ayrıca tedavi edilmelidir; örneğin asıl sebep akut bir barsak enfeksiyonu veya ishal ise; sadece antibiyotik ve ishal diyeti uygulaması bile yeterli olabilir. Cerrahi girişim gerektirmezler.
|

|
|
Resim 4:
Ikınınca kendini belli eden grade 2 hemoroid.
|
2) Grade II (2. Derece) hemoroidler: Bunlar dışkılama sırasında tuvalette ıkınınca anüs dışına çıkan ve ele gelen, ayağa kalkınca anal kanal içine çekilip kaybolan, ağrısız, 1 - 3 cm çapında Hemoroid memeleri olup, taharetlenirken genellikle püskürür tarzda veya hızlı damlalar şeklinde kanama yapar.Kanamalar bazan bir iki ay ara verebilir, bazan aylarca, her tuvalet çıkışında az da olsa görülür. Ve zaman içinde mutlaka kansızlık yapar ve bazan da aniden alevlenip büyüyerek anüs dışında kilitlenip kalarak acilleşebilir.
TEDAVİ:İkinci derece Hemoroidler yine cerrahi tedavi gerektirmezler. Bağlama, sklerozan ilaç enjeksiyonu veya infrared ışık koagülasyonu ile tedavi edilirler. Ayrıca uygun diyet, büzüştürücü ve antibiyotikli melhemler, ılık su oturma banyoları ve ağrı kesiciler tedaviye eklenmelidir.
|

|
|
Resim 5:
İtilmesse dışarda kalıp gittikçe morarıp, akıntı ve kanama yapan grade 3 hemoroid
|
3) Grade III (3. derece) hemoroidler: İç (internal) hemoroid memelerinin kolayca anüs dışına çıkması, sık sık pıhtı ve ödemle birlikte ağrı yapması, üzerinde iltihap ve aftlar şeklinde yaraların ve kanlı akıntının olması; içeriye itilmediği sürece anüs dışında kalması veya içeri geç çekilmesi halidir.
TEDAVİ:Tedaviye duruma göre önce tıbbi ve konservatif yöntemlerle başlanır; çok az vakada cerrahi eksizyon gerekir. Bunlarda en ideal yöntem lastik bant veya infrared koagulasyon uygulamaktır (Şekil I - II).
|

|
|
Resim 6: Eski hemoroid pakeleri ve içten gelen yeni hemoroid pakeleri, hastalığı alevlendirmiş.
|
4) Grade IV (4. derece) hemoroidler: Yıllarca süren kronik kabızlık hallerinde eski iç ve dış hemoroidlerin topluca aşağı sarkması, tuvalette veya koltukta çok oturma sonucu, memelerin büyük, ağrızsız, sulu, ıslak pakeler halinde anüs dışında çepeçevre yerleşip temelli kalmasıdır. Kronikleşmiş grade IV hemoroidli hastaların, iyi temizlenememe ve sürekli mukuslu ve iltihablı akıntılar, kaşıntılar ve az fakat sık sık kanama sorunları vardır. Memelerin üzerine oturunca hastanın canı yanar.
TEDAVİ: Pekçoğu iyi bir tıbbi tedavi, kabızlığı önleyici bol posalı diyet, düzenli tuvalet alışkanlığı gibi tıbbi ve hijyenik tedbirlerden kısmen yarar görürler. Bir kısmında lastik bant veya skleroterapi ve infrared ışık ile koagülasyonu yeterli olabilir; ancak çoğunda cerrahi tedavi endikedir; ancak cerrahiye engel varsa, ömür boyu, konservatif tıbbi yöntemlere devam eder ve daima bol su, bol sebze, bol meyva alırlar; asla çay, kahve, kola, rafine gıda ve baharat alamazlar.
HEMOROİD KOMPLİKASYONLARI
Hemoroid komplikasyonlarının başlıcaları:
a) Uzun süreli kanamalar sonucu anemi ve buna bağlı hipotansiyon, halsizlik, iştahsızlık ve solukluktur.
b) Memelerde yaralanma ve iltihaplanma sonucu lokal ve sistemik ateş.
|
 |
|
Resim 7:
Akut, tromboze hemoroid |
c) Strangulasyon, yani dışarda duran hemoroid memelerinin; stres, alkol, ağır yemek, kabızlık, mushil kullanımı ve ishal gibi bir nedenle aniden pıhtılarla dolması sonucu şişip tamamının anüs dışına fırlaması ve orada kilitlenip kalması, anormal şişmesi ve şiddetli ağrı yapması. Bu safhada hemoroid memelerinin kan dolaşımı bozulmuştur ve dolayısı ile nekroz ve şiddetli ağrı gelişir. Artık geriye itilemez ve el değmez ve dışkılamaya, fitil koymaya, hatta melhem bile sürmeye izin vermez; dışkılama ve günlük yaşam ve bütün işler engellenir; ağrı ve kanamalar, enfeksiyon ve ateş yüzünden halsizlik ve iştahsızlık gelişir. Hemoroidin en kötü şeklidir. Tedavi aciliyet gerektirir. Duruma göre önce konservatif tıbbi yöntemlerle başlanır. Gerekirse anında genel anestezi ve regional anestezi ile cerrahi eksizyon veya trombektomi, sistemik ve lokal antibiyotik uygulanır.
HEMOROİD VE SPASTİK KOLON HASTALIĞINDA DİKKAT EDİLMESİ GEREKENLER VE DİYET
1. Düzenli, dakik, kahvaltı ve tuvalet . Tuvaletten 5 dakikada çıkın.Gerekirse tuvalete günde 2 kez gidin.
2. Kahvaltı dahil her 3 öğünde,mutlaka bir tabak çoban salata yiyin.
3. Öğünlerinizde özellikle ıspanak, bamya, pırasa, semiz otu, yeşil fasulye gibi sebzeli yemekler. Mümkünse çorba, börek türü her şey sebzeli olsun
4. Her öğünde bir tabak dolusu hoşaf veya erik, incir, üzüm, kayısı gibi meyveler yiyin.
5. Tahıl,mısır ve baklagiller gibi lifli gıdalar ve kepekli ürünler tüketin.
6. Her yemekten sonra oda sıcaklığında bol ılık su için.
7. Her öğünde mutlaka Melisa çayı için ve Keten tohumu alın. Keten tohumunu herhangi bir tabak yemeğe bir tatlı kaşığı kadar katın.
8. Tuvalette aktif, hızlı kanama olunca hemen kalkın ve 10 dk uzanıp istirahat edin.
9. Çay, kola, muz, beyaz ekmek, sandviç, kurabiye ,gofret, çikolata, pirinç pilavı, makarna, su böreği vb. gibi posasız ürünleri kısıtlayın. Bunlardan illa da yerseniz, birlikte bol sebze, meyve de yiyin ve bol su için.
10. Soğuk içeceklerden uzak durun; içecekleriniz oda sıcaklığında su, erik, kayısı cinsinden olsun.
REFERANSLAR
1. Morinaga K,Hasuda K,Ikeda T.A novel therapy for internal hemorrhoids:ligation of the hemorrhoidal artery with a newly devised instrument (Moricorn) in conjuction with a Dopple flowmeter.Am J Gastroenterology 1995;90:610-3.
2. Sohn N,Aronoff J S,Cohen F S,Weinstein M A.Transanal hemorrhoidal dearterialization is an alternative to operative hemorrhoidectomy.Am J Surgery 2001;182:515-519.
3. Bursics A,Morvay K,Kupcsulik P,Flautner L.Comparison of early and 1-year follow-up results of conventional hemorrhoidectomy and hemorrhoid aretery ligation:a randomized study.Int J Colorectal Dis 2003 July 5(Epub ahead of print).
4.Shelygin IuA,Titov Aıu,Veselov VV,Kanametov MKh.Results of ligature of distal branches of the upper rectal artery in chronic hemorrhoid with assistance of Doppler ultrasonography.Khirurgiia(Mosk) 2003;1:39-44.
5. Arnold S,Antonietti E,Rollinger G,Scheyer M.Doppler Doppler ultrasound assisted hemorrhoid artery ligation.A new therapy in symptomatic hemorrhoids.Chirurg 2002 Mar;73:269-73.
6.Muller-Lobeck H.Ambulatory hemorrhoid therapy.Chirurg 2001 Jun;72(6):667-76.
|